Coming to terms with your emotion
In this section
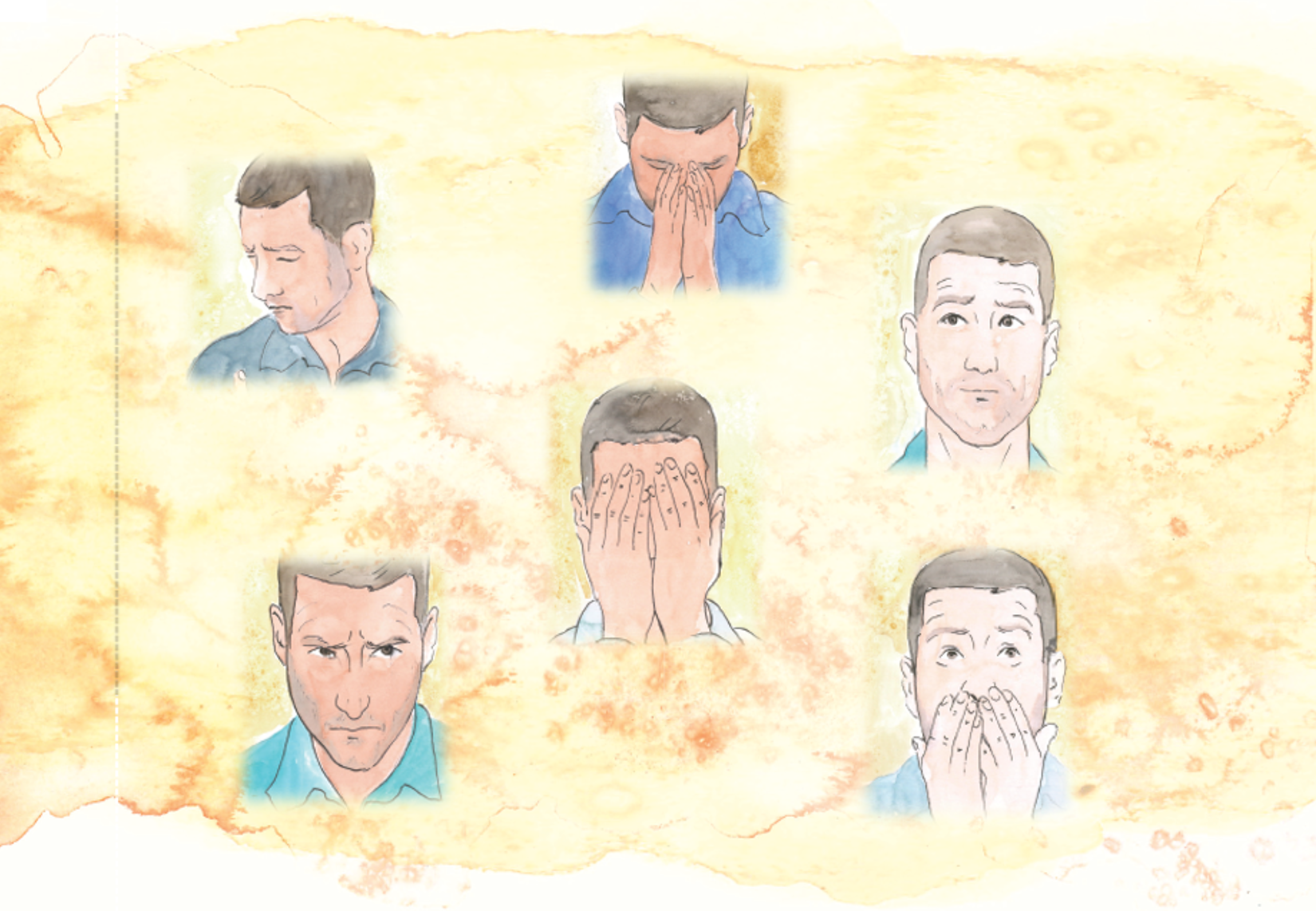
Providing care for a person with schizophrenia is a difficult job that requires a tremendous amount of time, energy, and dedication. Leaving aside daily struggles, caregiving can also bring to the surface A WIDE VARIETY OF EMOTIONS. Some of these emotions exist from the start, as many caregivers find themselves thrown into the role unexpectedly, and adjusting can be very stressful. Other emotions surface only after you have been caregiving for a while.
As a caregiver, you may experience both POSITIVE AND NEGATIVE EMOTIONS .
Some days, caregiving may provide a deep sense of fulfillment and connection, along with feelings of respect, empathy, joy, and gratitude. Other days it may bring feelings of guilt, anger, shame, fear, anxiety, loneliness, or disappointment. You may also feel frustration, impatience, lack of appreciation, jealousy, irritability, and being overwhelmed. There may be a possibility for conflicting feelings to arise such as love and resentment being experienced simultaneously; these emotions may appear in various ways on a daily basis.
Experiencing all these emotions can become GRUELING , and if not closely monitored, they
will wear you down. You may think that this will not happen to you because you love the person you take care of. But after some time, the negative emotions that we tend to bury come up. In the long term, they can take a toll on even the most dedicated caregivers, both physically and emotionally.
So how can you avoid burnout and feeling overwhelmed? It is essential for you to know that it is COMMON to experience a broad spectrum of emotions, including negative ones. Each and every one of your emotions about caregiving either positive or negative are perfectly reasonable and important, apart from being allowed and expected. Having all these emotions means that you are human. Do not try to avoid them. Ignoring your feelings and telling yourself that you must
stay “strong” for your loved one or for the whole family is not the answer. Most psychologists
agree that avoiding your feelings is not a sign of strength; actually, it takes more courage to face your emotions than to avoid them.
Coming to terms with your emotions is also HEALTHIER. Acknowledging and expressing
your emotions can make you physically and mentally more resilient to stress and infections. In contrast, holding your emotions inside can weaken your immune system and expose you to a greater risk for conditions such as heart disease, cancer, or diabetes. Not paying attention to your feelings, and especially to expressing them, can lead to poor sleep, overeating, substance abuse, depression, and anxiety.
UNDERSTAND YOUR EMOTIONS AND POINT THEM TO YOUR ADVANTAGE
Rather than avoiding your emotions, you can use them to learn new things about yourself
and your loved one. When you give yourself permission to have feelings and recognize that
your feelings do not control your actions, your negative emotions will either subside or be easier to handle. In the long run, this will enable you to provide better care for your loved one, but it will also help you to take care of yourself.
As every caregiving experience is different, there are NO “RIGHT” OR “WRONG” FEELINGS . In order to provide the best care possible, it is helpful to be familiar with the type
of feelings that could come about, ways of detecting them, and strategies of dealing with them.
The following strategies are aimed at helping you cope with complex emotions that are experienced by numerous caregivers on a daily basis.
Although caregiving is most of the time challenging, it can also be a REWARDING EXPERIENCE. Allowing yourself to experience positive emotions is not about pretending that things aren’t difficult or that you are not stressed. It is also not about pretending you are not experiencing negative emotions, because that is normal and valid. However, you can experience positive emotions alongside negative ones, even in great stress. Positive emotions have unique benefits, independent of the effects of negative emotions. By giving yourself the permission to FOCUS ON YOURSELF, even if it’s just for a few minutes a day, you will be able to enjoy the positive moments and not let caregiving take over every aspect of your life.
Experiencing positive, rewarding feelings has multiple benefits, for both you and your loved one, as they reduce the physical effects of stress and can make both of you live longer. Moreover, we are “hardwired” in a way that tending to the needs of others
helps reduce anxiety. Increasing the positive can help boost your reservoir of personal resources to cope better with your hardships and challenges. It can also make you a better caregiver and improve your relationship with the person you care for.
How to focus on positive?
Learning positive emotion skills can help you experience more positive emotions and reduce anxiety. Practicing these skills every day will take you a long way ahead to a rewarding journey as a caregiver.
NOTICE THE POSITIVE. Be mindful of the positive things present in your life rather than reducing your focus to the negative ones.
CAPITALIZE ON POSITIVE EVENTS. Savor your positive feelings by sharing them with others, making written notes of them, reminiscing on the event later.
PRACTICE MINDFULNESS. Be mindful of being present and disregard the judgement. You can incorporate mindfulness into the most basic daily activities like brushing teeth or washing dishes.
BE AWARE OF YOUR STRENGTHS. Acknowledging the personal resources you hold and how to make use of them in your life will greatly reduce the feeling of helplessness.
SET ATTAINABLE GOALS. Choose challenging goals, but not overly, just enough to allow you to experience accomplishment and success without getting overwhelmed.
Compassion
Compassion is a person’s ability to feel a sympathetic concern for another person’s suffering, usually accompanied by a strong desire to ease that suffering. Of all the things you do as a caregiver, establishing a COMPASSIONATE CONNECTION with your loved one is probably the most important. It is the essence of being a caregiver.
Compassion enables individuals to soften their hearts towards others and engage in honest communication. When caregiving is done with compassion, you build trust and form a deeper, more meaningful relationship with your loved one. For you, this can change the entire caregiving experience from challenging to rewarding. For them, it has a significant positive impact on their life quality.
There are many ways in which you can show compassion towards your loved one: through small acts of kindness, by truly dedicating your time to them, or by seeing the person behind the illness. But most importantly, by BEING PRESENT AND GENUINELY LISTENING.
Respect
The desire for respect and dignity is among our most important human needs. Although offering a loved one help with maintaining a sense of dignity counts, there are many things you can do to make sure that they get well-deserved respect.
RESPECT THEIR PRIVACY.
Most of the time, people with schizophrenia live in the same household as their caregivers. This has many advantages, but it can also increase their stress if they feel you invade their private space, you are overprotective, or try to run
every aspect of their lives. Besides their physical privacy, you should also respect their emotional privacy and not discuss confidential information with others without their permission.
RESPECT THEIR RIGHT TO MAKE CHOICES.
Let your loved one have a sense of control over their life by choosing what they wear or what they eat, for example. If you find it more helpful, try to offer several choices. If their choice is not important in your opinion, try to understand the reasons why it may be important to them. If you find their choice to be dangerous, try to encourage them by offering alternatives or negotiating possible solutions.
INVOLVE THEM IN DECISIONS RELATED TO THEIR CARE.
Taking decisions without involving your loved one is possible to make them feel disconnected and undervalued. Make sure they are part of the discussions that affect their care. This will increase their feeling of being valued and in control, and therefore their adherence to treatment.
LISTEN TO THEM.
Even if they have difficulties in expressing themselves, listen to their concerns, ask for their opinion, and try to include them in the conversation. Making your loved one feel respected lowers their distress and increases their comfort. Moreover, respect provides you with mutual understanding, facilitates better communication, and builds a stronger connection.
Gratitude
It can be hard to be thankful when every day seems to hold a new challenge. And that’s all right. Being grateful does not mean ignoring how hard caregiving can be. It is about finding something to be thankful for each and every day. When you are able to do that, you get a different perspective and the comforting thought that things are not bad all the time.
Gratitude can work wonders in restoring your well-being and has a multitude of benefits for your mental and physical health: it reduces stress, helps you sleep better, and boosts your immune system. Being grateful also helps you become more optimistic and focus on what you have instead of what you don’t.
In time, being grateful becomes a habit that improves your overall attitude. The best way to develop this habit is to keep a gratitude journal. Each day, write down at least one thing that made you feel grateful that day. Be mindful of both the small and the big things. When you are down or feeling stressed, read from your journal to boost your mood and shift your perspective.
Challenging feelings
Guilt
Guilt is probably THE MOST COMMON EMOTION you may feel as a caregiver.
We all experience guilt when we do something wrong. When taking care of a person with schizophrenia, guilt can come from a variety of sources. However, it is usually related to the fact that caregivers tend to blame themselves when something goes wrong.
The guilt that caregivers experience has a multitude of facets:
guilt that they are not doing enough or they should be better at it;
guilt that they are not spending enough time with the person they take care of;
guilt that they are not spending enough time with their family;
guilt that they are not taking care of themselves;
guilt that they make their own well-being a priority;
guilt that they are unfocused at work because of caregiving;
guilt that they care about their career when they have others to care for;
guilt for moving their loved one to an institution or assisted living;
guilt over not taking enough action to prevent the illness to begin with;
guilt over having the desire for this to disappear;
guilt over all the negative emotions they experience.
The reason why guilt is so common among caregivers is that they often overwhelm themselves with a great deal of “oughts”, “shoulds”, and “musts” devised by their own self. They often have a pretty clear picture of how they should behave or act, and feel guilty when they do not succeed in acting accordingly. However, this picture is not always accurate. As a consequence, guilt often arises when there’s a mismatch between their day-to-day choices and what they think the “ideal” choice would have been.
Whatever the source, guilt can be a particularly destructive emotion if you are blaming yourself due to mistakes that are most likely either presumed, exaggerated, or purely human.
How to cope with guilt
First of all, learn to forgive yourself. You cannot be perfect, and you cannot be in control all the time. Even with your best intentions, your time, skills, energy, and resources are limited. So go easy on yourself and provide the best care that you can while allowing yourself to be imperfect.
Second, lower your standards and set realistic limits to what you can accomplish. Instead of feeling guilty for not doing enough, look at the other way and appreciate the difference you are making every day in the life of the person you care for. Understand and accept your limits. Otherwise, you risk facing caregiver burnout.
Whenever you experience the feeling of guilt, it is worth asking yourself what might have triggered it. A firm “ought”? An exaggerated belief of your capabilities? Most importantly, you must recognize that guilt is unavoidable and get comfortable with not obtaining perfection.
Shame
Shame can be described as one’s terrible feeling of embarrassment brought on by the realization of their own inappropriate behavior or actions. Shame is usually triggered by not aligning to social standards, and it is fueled by the fear of being socially excluded.
Although we often use the words “guilt” and “shame” interchangeably, there is a clear distinction between the two feelings. While guilt reflects how you feel about your actions, about what you did (or did not do) to another person, shame reflects how you feel about yourself. Shame is a painful feeling about how you appear to others, and it is not related to your actions.
As a caregiver, the guilt you may feel stems from the stigma connected with schizophrenia, which manifests itself as criticism or animosity from people who don’t understand it. At the same time, your shame may be fueled by your own prejudices and lack of knowledge about the illness. The parents of young adults with schizophrenia often feel shame thinking that the illness could have been prevented had they been better parents.
Whatever the cause, shame leads to avoidance and isolation from friends, family, and society in general. But what is worse, shame also leads to avoidance of treatment: the families of people with schizophrenia are often reluctant to seek help to avoid feeling trapped and embarrassed.
In the long term, shame HAS A NEGATIVE EFFECT ON THE QUALITY OF YOUR LIFE,
increasing the risk of depression and anxiety. Such an undesirable event can also have a negative impact on your relationship with the person you care for. In the worst case, it can lead to the development of an unpleasant environment for your relationship that will only worsen your loved one’s symptoms.
How to cope with shame
The most important way you can deal with the shame caused by stigma is to educate yourself and others. Learning about the illness and spreading the knowledge will help reduce the stigma and will have a beneficial effect on you, the person you care for, and the people in your personal environment.
As for the shame you may feel as a parent, you need to stop blaming yourself. The theories that put the blame on the parents when a young adult was diagnosed with schizophrenia have crippled many families with feelings of guilt and shame, but time has proven that they were wrong. According to our current understanding of the illness, there is nothing you could have done as a parent to prevent it.
You must accept that no matter the connection or the relationship you share with the person you care for, you cannot control their behavior. What is in your power to do is to accept this reality and to be compassionate towards them. This way it is possible for you to cure yourself of the shame.
Anger
Anger is probably THE SECOND MOST COMMON EMOTION you experience as a caregiver. There are many situations that can lead to feelings of anger:
seeing your loved one struggling;
seeing that your loved one is irrational or combative;
thinking about the future that both you and your loved one had to give up;
feeling trapped in a situation you were thrown into unexpectedly;
feeling that you are not appreciated enough for your everyday effort as a caregiver;
feeling that the person you take care of does not accept your help.
In these circumstances, it is not always possible to keep your emotions under control. You might say things you don’t mean or lose your temper. And while anger is a natural response given the hardships of being a caregiver, it can negatively impact both your relationship with the person you take care of and your health.
Chronic anger and hostility have been associated with high blood pressure, heart disease, digestive tract disorders, and headaches. Unexpressed anger that is built up over time can promote depression or anxiety, while explosive anger projected onto others may compromise relationships as well as cause them suffering. Managing anger does not only help with improving personal wellbeing, it also minimizes the likelihood of taking out the anger on a loved one.
How to cope with anger
Instead of avoiding anger, try to express it in healthier ways. Take the energy that comes with anger and try to channel it towards a positive experience. Ask yourself whether there may be a practical fix to the circumstances that anger you. Is a compromise possible? Would being more assertive (i.e., getting your point across firmly, fairly, and with empathy) help you feel a sense of control?
When you find yourself in a situation that angers you, try to remember the good times. Sometimes laughing at the absurdity of a situation can be a healthier way to let off steam than snapping. Another way to decrease anger, although a more difficult one, is to try to come to terms with the fact that your life has changed.
Most importantly, if you say or do something when you are angry, forgive yourself. Walk away and take a deep breath to regain your focus. Find constructive ways to express yourself, or talk to someone that you trust about what got you angry.
Resentment
Resentment is feeling bitter when you think you are being treated unfairly. In certain aspects, resentment is similar to anger. However, while anger is a sudden emotion, a reaction, resentment is a feeling of bitterness experienced when we let anger persist. Anger is natural; resentment is a choice. Thus, being resentful is choosing to keep the anger. It is reliving a hurtful experience over and over again. And while anger can sometimes be positive because it gives you the power to change things, resentment holds you back and can only hurt you and the person you care for.
Becoming the caregiver of a person with schizophrenia often means being suddenly placed in a situation that you didn’t choose and taking on an enormous task that you were not prepared for. In these circumstances, it is quite common to feel pessimistic and resentful. Because of the extensive amount of time spent on taking care of your loved one, IT IS REASONABLE TO FEEL RESENTMENT AS A CAREGIVER – despite the amount of love or care you have for them. For instance, it may be that you experience resentment towards the overall situation, the illness, specific behaviors, uncooperative family members, or friends who don’t offer much support. You may also resent your loved one, especially when their negative symptoms prevent them from showing compassion towards you.
How to cope with resentment
Being resentful actually requires a lot of energy, and you can redirect this energy in positive ways in order to find the silver lining. When you feel resentment towards your loved one, remember that many of your interactions are dictated by their disease. Their apparent lack of motivation and unwillingness to talk are symptoms of the illness that they cannot control.
Give your feelings some space by talking about your emotions with friends or family members. Be proactive in communicating with your loved one and everyone involved in their care; avoiding uncomfortable conversations will only add to your frustration and resentment. You can also use physical activity to move past the stuck emotional energy that usually accompanies resentment.
Most importantly, make the conscious decision to spend time on your own needs. If you don’t take care of yourself, the resentment will not go away, but it will continue to build.
Fear and anxiety
Caregiving anxiety is often a result of facing the unknown, or feeling out of control and not knowing how to regain it. There are many aspects in the life of a person with schizophrenia that can cause fear and anxiety. You may feel frightened of making significant mistakes or being confronted with issues you are not aware of how to solve. You may be afraid that something happens to your loved one when you are not by their side. You may also be worried about your loved one losing their job, or about you losing yours. Also, seeing your loved one in an altered or uncomfortable state typically produces feelings of stress and confusion. As a caregiver, you may EXPERIENCE ANXIETY IN MANY WAYS,
from having difficulty sleeping or feeling an impulse to run away, to having heart palpitations and feeling an urge to cry.
How to cope with fear and anxiety
The most effective way of dealing with fear when taking care of someone with schizophrenia is to educate yourself and try to plan in advance. Talk to the healthcare team treating your loved one and find out what to do in specific situations. Plan for every situation or crisis that may arise by finding the right balance between being prepared and being overprotective. Focus on the things you are able to have under control and make a contingency list of actions in case you are not nearby. Reaching out to others who are in a similar situation, for example through a support group, can also reduce stress-related anxiety.
It is important to be mindful of anxiety; it is your body’s way of signaling a potential threat. In case of experiencing anxiety, pause for a moment, focus on your breathing and take some time off from what is happening at the moment.
Isolation and loneliness
Despite the fact that you spend a great amount of time with the person you care for, YOU MIGHT FIND YOURSELF EXPERIENCING FEELINGS OF LONELINESS. And the longer you are a caregiver, the higher the risk of becoming isolated. With no one to talk to all day except the person you take care of, it is easy to lose a sense of yourself.
Relationships with friends may suffer because of your intense schedule or because they feel less wanted. You may hesitate to reach out and spend time with them because you feel that your life is all about caregiving and you have nothing to talk about or they do not want to hear about your struggles anymore. When taking care of a person with schizophrenia, the feeling of having lost your loved one’s companionship may also add to your isolation.
In the long run, the feeling of loneliness can have a negative impact on your health. It weakens your mental strength and makes you more prone to start having harmful habits like overeating, smoking, or abusing alcohol. Furthermore, social isolation is a risk factor for dementia.
How to cope with isolation and loneliness
The key to removing yourself from isolation is to sustain healthy relationships aside from your role as a caregiver. Find means of getting out of the house and engaging in other things besides caregiving. Find activities, such as sports or hobbies, that enable you to engage with individuals who can provide a feeling of belonging and support.
If getting out is troublesome, it might be worth reaching out to and inviting old friends over. Consider joining support groups concerned with your loved one’s illness or caregiving in general. Alternatively, you can find kinship with individuals who share your experience in online support groups.
Helplessness
Being the caregiver of a person with schizophrenia provides MANY OPPORTUNITIES FOR YOU TO FEEL HELPLESS, especially at times when you do every single thing in your power in order to help the person you care for and they are not getting better. Beyond your caregiving challenges, the emotions we talked about in this chapter can also make you feel helpless and unable to continue to be a caregiver. The feeling of helplessness can negatively impact your emotional health, leading to irritation, guilt, and even depression if this feeling persists.
How to cope with helplessness
When you are feeling helpless, ask yourself the following questions:
Am I having unreasonable expectations?
Do I know enough about how to solve this problem?
Am I getting enough sleep?
Am I taking care of myself?
It is important for you to realize that by doing the best you can, you are of invaluable help to your loved one. You also need to remind yourself frequently that their health is often beyond your control. Acknowledging your limits will allow you to pinpoint what is it that you are able of controlling, as well as redirect your energy. Reach out to friends or family and delegate some of your caregiving tasks. Also, make sure to get enough sleep and have some time for yourself. Being constantly tired increases your stress and the feeling of helplessness.
When faced with a complex problem, breaking it down into smaller, more manageable tasks can help you find the solution and avoid the feeling of helplessness. You can also cope with this difficult feeling by learning as much as you can about the illness and communicating frequently with the medical team treating your loved one.
Depression
It frequently happens that the caregiver’s attempt to offer their loved one the best possible care might be detrimental to their own physical and/or emotional needs. However, the stress of caregiving, the uncertainty of the future, as well as all THE NEGATIVE EMOTIONS LISTED ABOVE CAN TAKE A TOLL ON THEIR WELL-BEING AND LEAD TO DEPRESSION AND MOOD PROBLEMS. Studies show that as many as half of caregivers of people with schizophrenia have depression, particularly in cases where the illness is resistant to treatment.
People experience depression in different ways, as a change in symptoms can occur in time. If the occurrence of the following symptoms is persistent over the course of more than two consecutive weeks, it may be assumed that depression is present:
a change in eating habits leading to undesired weight gain or loss;
a change in the sleeping pattern (excessive or insufficient sleep);
experiencing constant tiredness;
a lack of interest in individuals and/or activities that were previously pleasurable;
experiencing anger and agitation at a much faster rate;
having the feeling of not being or doing good enough at anything;
suicidal tendencies or thoughts of death, or attempting suicide;
consistent physical symptoms which are unresponsive to treatment, for example, digestive issues, headaches, and chronic pain.
How to cope with depression
Depression is treatable and should be taken seriously. The attentiveness to symptoms in good time may help restrain the formation of a more severe depression case in the long term. Talk to your physician or a mental health professional if you suspect the presence of depression. Furthermore, physical activity and social interactions are excellent ways of dealing with sadness and depression as they create a way to alleviate tension, improve your mood, develop social relationships and boost your energy.
How to recognize emotional fatigue?
Emotional fatigue is a state of feeling emotionally worn out and drained as a result of the stress accumulated from caregiving. Emotional fatigue affects a large proportion of caregivers, and it is one of the signs of burnout.
Initially, the symptoms of emotional fatigue come and go; they may also be insidious or overlap with each other. They include:
nervousness or tension;
feelings of frustration, anger, or guilt;
feelings of resentment, impatience, and/or irritability;
feelings of sadness, hopelessness, and isolation;
forgetfulness, inability to concentrate, and/or mental sluggishness;
lack of motivation;
change in appetite;
poor or interrupted sleep;
heart palpitations;
increase in aches, pains, and blood pressure.
Your emotions in different stages of the disease
Your loved one’s symptoms and the course of the illness may set the tone for the different types of feelings you are faced with in different stages of the disease.
The first psychotic episode (The prodromal phase)
The first episode of schizophrenia is a CHALLENGING INTERVAL OF TIME THAT REQUIRES ACCEPTANCE AND ADJUSTMENT by the patients, as well as their families. For people who were just diagnosed with schizophrenia, it is a personal crisis associated with fear, guilt, shame, and hopelessness. For their family members, who were suddenly placed in a situation that they did not choose, it is a period of SHOCK, GUILT, SHAME, FEAR, ANXIETY, AND UNCERTAINTY.
The active phase
In the active phase of the illness, there is a predominance of positive symptoms such as hallucinations, delusions, and bizarre behavior. Almost all people with schizophrenia experience these symptoms at some point during the disease. In some cases, they appear only during the relapses. However, in almost half of cases, positive symptoms are present either most of the time or continuously.
Your loved one’s positive symptoms CAN HAVE A NEGATIVE IMPACT ON YOU, especially when they are not aware of them. They may say things that don’t make sense or accuse others of conspiring against them or stealing their thoughts. They may also see things or hear voices that frighten them. These symptoms may lead to verbal or bizarre behavior and put pressure on the entire family, leading to feelings of tension, frustration, and anxiety. The most common feelings and thoughts that caregivers experience in this period include the FEAR THAT SOMETHING WILL HAPPEN TO THEIR LOVED ONE, the fear of being subjected to violence, the idea that they may also have the illness, uncertainty, and hopelessness.
The residual phase
In the residual phase, when psychotic symptoms are subdued, there is a predominance of negative symptoms, such as avolition (the lack of drive or purpose), alogia (the reduced ability to speak), or blunted affect (the reduced ability to express emotions), and cognitive symptoms such as problems with attention, concentration, and memory.
In this period, for the family of a person with schizophrenia, ONE OF THE MOST FRUSTRATING SYMPTOMS IS AVOLITION. It is very difficult for them to see their loved one not having an interest in even the most basic daily activities. Many family members believe that the person they care for is able to influence their avolition. In this regard, they see their loved one’s inability to get dressed or to go to an appointment as laziness. As we’ve talked about this in previous chapters, avolition is a symptom of the illness, and as such, your loved one cannot influence it directly.
The most common feelings that you may experience in the residual phase are ANGER, FRUSTRATION, IRRITABILITY, IMPATIENCE, LONELINESS, LACK OF APPRECIATION, AND BEING OVERWHELMED. And because people with schizophrenia often have difficulties finishing their studies or getting a job, it is also a period of intense worry about your loved one’s future. In many regards, for you, the caregiver, the residual phase is even more challenging than the active phase. During the psychosis, even if the symptoms and events are frightening, you have some kind of interaction with your loved one. After the psychosis, families often expect things to return to normal and are waiting to get their loved one back. Instead, because of the negative symptoms, what follows is a period with fewer emotions and interaction from your loved one, which may lead to resentment and the feeling that your efforts as a caregiver are not appreciated.
Although we’ve talked mostly about challenging feelings related to the different phases of the disease, do not forget that in every phase of the disease, you can experience love, respect, and empathy, feelings that make your caregiving experience rewarding.
Emotionally-charged behaviors
In all phases of the illness, you may be faced with situations with a high emotional burden that TESTS YOUR CAREGIVER ABILITIES AND YOUR RELATIONSHIP WITH YOUR LOVED ONE. HOSTILITY, VIOLENCE, AND AGGRESSION. People with schizophrenia are not usually aggressive or violent. However, in some cases, the severity of the illness, alcohol or drug abuse, or the stress and frustration caused by the disease may cause your loved one to become aggressive or even violent. Violence is also associated with more severe symptoms, lower family income, and unemployment. Other times, your loved one may exhibit hostility toward you, or blame you for everything from imposing limits on them to getting the disease in the first place. In these situations, YOU NEED TO REMAIN CALM and REMEMBER THAT WHAT YOU SEE IS NOT THE PERSON YOU LOVE BUT THE ILLNESS.
For them, schizophrenia is a painful journey riddled with fear, anxiety, crippling symptoms, stigma, and the sense of an ever-changing reality.
SUICIDAL THOUGHTS. The symptoms of schizophrenia, stress, and depression may also lead to suicidal thoughts. These acute situations can be a deeply tense and emotional time for the entire family. You can FIND MORE INFORMATION on what to do if your loved one intends to hurt themselves in CHAPTER 6 OF THIS GUIDEBOOK.
REJECTION OF TREATMENT. People with schizophrenia often reject medication or other treatment options. This can happen for a number of reasons: they are not aware of their illness (anosognosia), they are feeling better, or conversely, they are feeling worse because of medication side effects. Because of all these reasons, they may also reject hospital admission. Anosognosia can cause a great deal of frustration for the entire family, but most often it improves over time. The best solution in these situations is to TRY TO UNDERSTAND THE CAUSE BY SEEING THE WORLD THROUGH YOUR LOVED ONE’S EYES. Talk to the healthcare team to find solutions that will help your loved one stick to their treatment.
SPECIALIZED TREATMENT FACILITY. The severity of your loved one’s illness may require long-term care that is only available in a specialized treatment facility. Dealing with the fact that your loved one can no longer be taken care of in the family can be particularly challenging emotionally. Make this decision together with everyone involved in their care, making sure to ACT IN THE BEST POSSIBLE INTEREST OF YOUR LOVED ONE, BUT ALSO YOUR FAMILY.
Manage tough emotions healthily
As strange as it may sound, caregivers often DO NOT REALIZE THAT THEY ARE CAREGIVERS. When their child, parent, or other family member is diagnosed with schizophrenia, they help out, because it is the right thing to do. The sooner you self-identify as a caregiver, the sooner you will be able to recognize and deal with the emotional roller-coaster that is caregiving. You will also recognize the emotional weariness that you will inevitably experience and start looking for ways to manage it.
The emotions we talked about in this chapter are often warning signs from your body; little reminders for you to pay attention and remember that YOU ARE IMPORTANT, TOO.
These emotions can be experienced by every caregiver. Admitting this will help you take care of yourself and not react to them in a negative way. You also need to understand that what causes your emotional fatigue the most is out of your control. Be aware of your limitations and let go or delegate some of the responsibilities. The key to being a successful caregiver is FLEXIBILITY AND ADAPTABILITY on the journey.
Most importantly, remember that NOBODY CAN DO THIS JOB ALONE. Get help, even from the earliest stages of caregiving. It will significantly increase your well-being, and it will enable you to provide the best care you envision for your loved one.
References
- How to Handle Guilt and Other Caregiving Emotions [Internet]. WebMD. [cited 2021 Mar 21]. Available from: https://www.webmd. com/healthy-aging/caregiver-overcome-guilt
- Ong AD, Mroczek DK, Riffin C. The Health Significance of Positive Emotions in Adulthood and Later Life. Soc Personal Psychol Compass. 2011 Aug 1;5(8):538–51.
- Mund M, Mitte K. The costs of repression:a meta-analysis on the relation betweenrepressive coping and somatic diseases.Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2012 Sep;31(5):640–9.
- Kamil SH, Velligan DI. Caregivers of individuals with schizophrenia: who are they and what are their challenges? Curr Opin Psychiatry. 2019 May;32(3):157–63.
- Newman KM. How Caregivers Can Cultivate Moments of Positivity [Internet]. Greater Good. [cited 2021 Apr 26]. Available from: https://greatergood. berkeley.edu/article/item/how_caregivers_ can_cultivate_moments_of_positivity
- Poulin MJ, Brown SL, Dillard AJ, Smith DM. Giving to Others and the Association Between Stress and Mortality. Am J Public Health. 2013 Jan 17;103(9):1649–55.
- Tangney J, Tracy J. Self-conscious emotions. In: Leary M, Tangney J, editors. Handbook of self and identity. The Guilford Press; 2012.
- Chan SW. Global perspective of burden of family caregivers for persons with schizophrenia. Arch Psychiatr Nurs. 2011 Oct;25(5):339–49.
- Miller R, Mason SE. Shame and Guilt in First-Episode Schizophrenia and Schizoaffectiv Disorders. J Contemp Psychother. 2005 Jul 1;35(2):211–21.
- De Rubeis S, Hollenstein T. Individual differences in shame and depressive symptoms during early adolescence. Personal Individ Differ. 2009 Mar 1;46(4):477–82.
- Anger — how it affects people | betterhealth. vic.gov.au [Internet]. Better Health. [cited 2021 May 1]. Available from: http:// www.betterhealth.vic.gov.au/health/healthyliving/anger-how-it-affects-people
- Sundström A, Westerlund O, Kotyrlo E. Marital status and risk of dementia: a nationwide population-based prospective study from Sweden. BMJ Open. 2016 Jan 4;6(1):e008565.
- Bademli K, Lök N. Feelings, thoughts and experiences of caregivers of patients with schizophrenia. Int J Soc Psychiatry. 2020 Aug;66(5):452–9.
SCHIZOPHRENIA: MYTHS vs TRUTHS
You might already have some preconceptions about schizophrenia, but do you know the myths from the truths? Explore common myths about schizophrenia and the trut
more…Бред или паранойя: какая разница?
Паранойя и бред — это термины, применяемые в психиатрии. Они означают состояния, которые часто переплетаются при развитии психических заболеваний
more…