The 3 A’s of stigma remedy:
Acknowledge, Apprehend, Alleviate
In this section
You are not alone!
There are more than 20 MILLION people living with schizophrenia around the world. By their side are the caregivers who face the same fears, difficulties, and challenges as you are right now. Get in touch with them. Join a support group or a caregivers association. There is a large network of caregivers in Europe who share the same goal: to positively impact the lives of those they care for.
This can also give you the opportunity to connect with other families affected by schizophrenia. People with schizophrenia and their families often feel isolated or misunderstood. You may find it helpful to connect with them and exchange experiences and advice.
Most importantly, talk to healthcare specialists. If there is a medical team taking care of your loved one, turn to them for advice. Become actively involved in the conversation. Remember: YOU ARE NOT ALONE!
– Mrs. A. J., mother of a young man with schizophrenia
First steps
Finding out that your loved one is diagnosed with schizophrenia can be one of the most daunting experiences of your life. You may feel that you are suddenly given a role you are not prepared for. You may experience feelings such as shock, anger, fear, frustration, guilt, and anxiety. You may also feel helpless, worried, confused, and embarrassed.
It is important to keep in mind that we have come a very long way in our understanding of schizophrenia. Today, with the right treatment and support, WE ARE ABLE TO MANAGE THE DISEASE AND HELP PEOPLE WITH SCHIZOPHRENIA take back their place in society and live a gratifying life. As a caregiver you are very important in the life of person with schizophrenia you care for. The first step in providing the support they need is accepting the diagnosis and understanding your own thoughts and emotions. In this process, it is very important to recognize that some of the negative thoughts you may have about schizophrenia are caused by the stigma associated with it.
–Mrs. A. J., mother of a young man with schizophrenia
Stigma and its raison d’être
What is stigma?
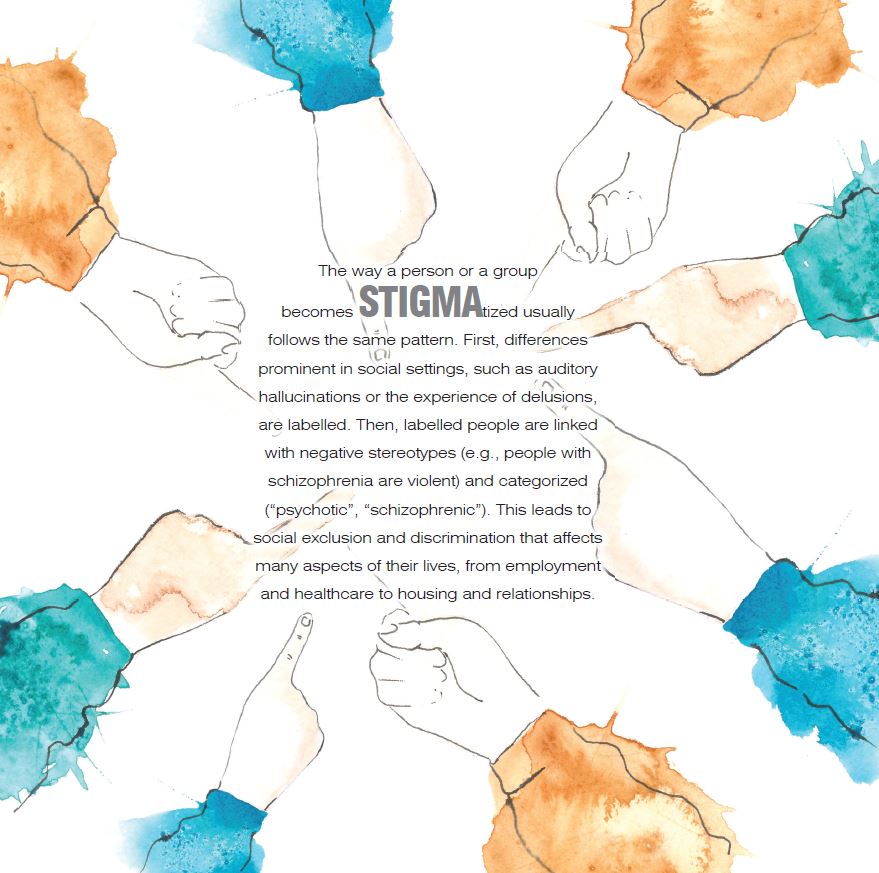
In Ancient Greece, the term “STIGMA” was used for the marks pricked into the skin of slaves. These marks signaled that they are someone’s property and have inferior social status. In our days, STIGMA represents something similar: we, as a society, mark a person for having a mental illness, a health condition, or a disability. We label them as inferior or threatening. As a result, they have to face negative attitudes in the form of prejudice, and negative behavior in the form of discrimination.
There are three types of STIGMA:
INTERPERSONAL STIGMA or SOCIAL STIGMA refers to the negative attitudes of society towards STIGMAtized individuals. These attitudes are caused by feelings of anger, anxiety, pity, or fear and result in the social rejection and isolation of the STIGMAtized person.
Example: “I’d like to invite everyone from the office to my party, but I’m afraid if poor George comes, he will make everyone feel awkward with his mental problem.”
INTERNALIZED STIGMA or SELF-STIGMA develops when stigmatized individuals believe the negative assumptions that society has about them. They internalize negative stereotypes and view themselves as flawed compared to others, which leads to emotions of embarrassment, shame, fear, and alienation. These feelings act as a barrier, keeping them from seeking support, employment, or treatment. Example: “Someone like me, a mentally ill person, is dangerous for their family. I will not even try to have a family.”
INSTITUTIONAL or STRUCTURAL STIGMA refers to situations where the policies established by institutions of either private or governmental nature limit, often invisibly, the opportunities of those experiencing mental illness (e.g., they have difficulties obtaining health insurance coverage, or they are unable to vote or hold political office).
Although many health conditions are affected by STIGMA, mental illnesses seem to attract the most negative associations. People with schizophrenia are often targets of negative attitudes and social labels that lead to STIGMA. The reason is that there is still a lot of misunderstanding surrounding schizophrenia. Many people assume that it means having split personalities or being violent, neither of which is true.
Historically, there is a persistent case of stigmatization around mental illness in our society. There was a wide range of beliefs regarding the cause of mental illness, from being regarded as the devil’s mark to being accounted as a divine punishment.
The mentally ill were considered at best unable to pursue a life in society and at worst a menace to it. This belief has remained consistent over numerous centuries and it has only started to be disputed fairly recently. In the last decades, we’ve learned a great deal about how these conditions develop and how they can be treated. In spite of this, the STIGMA of mental illness is still widespread, and many people continue to negatively view individuals with mental health conditions.
The stigma impact
STIGMA constitutes one of the major challenges that individuals experiencing mental illness have to face. In many cases, it is even worse than the symptoms of the illness itself. “IN FACT, I SUFFER FROM TWO DISEASES, SCHIZOPHRENIA AND THE STIGMA OF SOCIETY.” Regarding people with schizophrenia, stigma can affect not only their place in society but also their physical and emotional well-being. Thus, they have to endure not only the illness but also the negative attitudes that society attaches to them.
The social impact of STIGMA affects every life aspect of a person with schizophrenia. Prejudice and discrimination exclude them from activities that are open to other people. This limits their ability to get and keep a job or a safe place to live or get healthcare and support. It also limits their ability to make friends or have long-term relationships, or take part in social activities.
One important attribute of the social impact of STIGMA is that it is long-lasting. An episode of sychosis that is well treated may leave no trace and may never return. However, the STIGMA of the disease may last a lifetime. It may even have repercussions for the children of the person who experienced a stigmatizing illness.
STIGMA also has a direct impact on the health of people with schizophrenia. It causes them to question themselves and their capacity to achieve their life goals. Stigma increases feelings of isolation, resulting in decreased self-esteem as well as feelings of despair. These effects are vulnerable to the enhancement of the symptoms. After years of persecutory delusions and commenting voices, people with schizophrenia have little sense of their own worth or their capabilities.
SELF-STIGMA leads to isolation and a series of other negative effects: stigmatized persons tend to avoid or delay seeking treatment, perceive the need for treatment as a sign of weakness, and have trouble following the treatment. STIGMA can also influence how the illness progresses: it can precipitate initial episodes of psychosis, trigger relapses, and result in a more severe disease course.
I realize that I have become very insecure about what I can trust myself to do, that I often lack self-esteem, that I should apply for a job, or that I am more and more insecure in my interactions with others. I am afraid of coming across as strange, therefore I avoid other contacts and see only my family.”
–L. J., young man with schizophrenia
What keeps stigma alive?
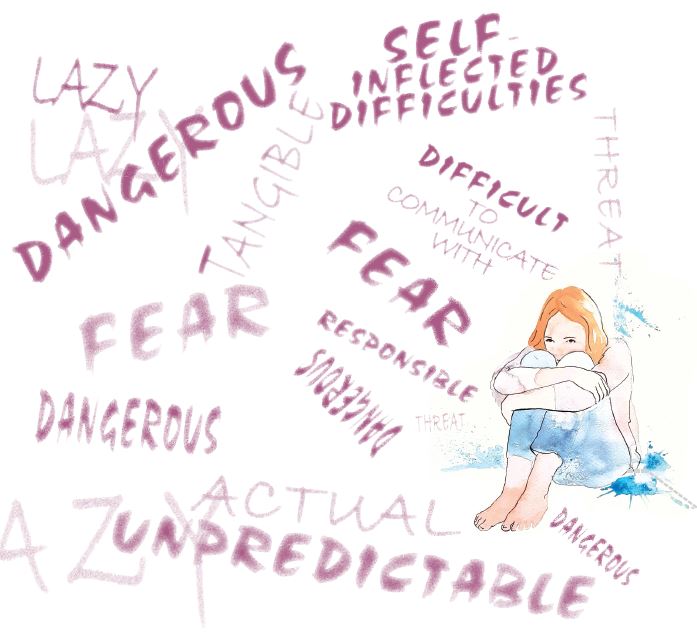
Although we know more about what stigma is than why it develops, studies suggest that one of its main driving forces is fear. Society perceives mental illnesses as a threat, both to
its core values and material goods.
One of the most common stereotypes is that individuals living with a mental disease hold responsibility for their condition. As a result, their inability to secure or keep a job is seen as laziness, and society does not tolerate laziness. In this regard, mental illness is considered a symbolic threat to society’s beliefs, values, and ideology. The other common stereotype is that those with a mental illness are erratic and dangerous. Thereby, they are seen as an actual, tangible threat to personal security. In this context, prejudices serve as a form of self-protection.
Another reason why mental health stigma exists is ignorance. Although we have an unprecedented volume of information at our disposal, our level of knowledge about mental illnesses is insufficient.
The most popular beliefs – people who suffer from mental illness are dangerous, their difficulties are self-inflicted, and they are difficult to communicate with – all come from a lack of knowledge.
Stigma is also deeply rooted in our inability to accept people who deviate from what we consider “normal”. This can be related to their skin color, their cultural or religious beliefs, or even the way they dress. In the case of schizophrenia, it may be related to the way they see the world or how they act because of the disease. People who are different (i.e., are not part of the same social group as we are), are usually prejudiced. By definition, prejudice is a preconception that is not founded on reason or genuine experience. In some instances, prejudices are actually useful. For example, we are wired to rapidly appraise the surrounding environment and construct quick assumptions and generalizations. Such generalizations are vital as they enable us to foresee, simplify, and categorize our world. The problem occurs during the assumption of unfair negative beliefs on particular individuals or groups of them, and the categorization of “them” as possessing alike characteristics.
The media also has a significant role in mental health stigma. News reports often perpetuate harmful stereotypes by linking mental illness with violent behavior or depicting individuals with mental health issues as dangerous, criminal, vicious, or disabled.
Myths and misconceptions about schizophrenia
“PEOPLE WITH SCHIZOPHRENIA ARE VIOLENT OR DANGEROUS.”
Due to the way they are depicted in literature or media, people with schizophrenia are considered volatile or dangerous. However, the vast majority are not violent. On the contrary, they are often the victims of violence due to their strange behavior and the fear they elicit in others. There are exceptions, of course. People who have untreated schizophrenia may become more violent over time, and alcohol and drug abuse may also lead to more aggressive behavior.
“SCHIZOPHRENIA IS PURELY GENETIC.”
There is a strong genetic component in schizophrenia, and the illness tends to run in families. However, genes are only a small part of the picture, as identical twin studies have shown. While we do not know exactly how schizophrenia develops, our current understanding is that it is caused by a complex interaction between genes and a series of other factors that include stress, hormonal changes, and drug abuse.
“SCHIZOPHRENIA IS THE RESULT OF BAD PARENTING.”
Bad parenting was believed to cause schizophrenia for a big part of the 20th century.
It was thought that traumatic experiences in early childhood led to the occurrence of schizophrenia in teenagers. Mothers, in particular, were blamed. The theory was damaging for both the patients and their families, contributing to social stigma. It also induced feelings of guilt and did not help understand the disease. Although childhood abuse can be a risk factor, there is not any evidence that it causes schizophrenia directly.
“SCHIZOPHRENIA ONLY INVOLVES HALLUCINATIONS.”
People with schizophrenia often have hallucinations and delusions. However, they are not the only symptoms of the illness. Other symptoms include lack of motivation, disorganized speech, or reduced ability to express emotions. The misconception is probably explained by the fact that hallucinations are much more visible and can have a larger impact on people who are not familiar with them.
“MEDICATION FOR SCHIZOPHRENIA ARE JUST TRANQUILIZERS.”
Early antipsychotic medication had certain side effects that caused people to become sedated and more lethargic. These antipsychotics were misleadingly called “major tranquilizers”, and the term continues to be used, leading to confusion. With the development of modern treatments, these side effects have diminished greatly. Currently used antipsychotics are increasingly specific and selective.
“PEOPLE WITH SCHIZOPHRENIA MUST BE HOSPITALIZED.”
Owing mostly to media portrayals, it is a common misconception that people with schizophrenia need to be hospitalized for long periods of time. As a matter of fact, thanks to advancements in treatment possibilities, schizophrenia was deinstitutionalized in the 1950s.
As a result, increasing numbers of patients are treated at home. Although the disorder can be debilitating, and hospitalization may be needed for certain periods, with treatment, people with schizophrenia can function well in their daily activities and can live a rich, meaningful life.
“PEOPLE WITH SCHIZOPHRENIA MUST BE HOSPITALIZED.”
“SCHIZOPHRENIA MEANS HAVING MULTIPLE PERSONALITIES.”
This is one of the most common schizophrenia-related myths. The confusion seems to originate from the Greek word schizophrenia, meaning “split mind”. However, the term actually refers to a split between thoughts, emotions, and behavior. There is also a misconception that the voices heard by people with schizophrenia are coming from other personalities within them. Although schizophrenia alters the way they think, it does not mean multiple personalities.
The power of knowledge
One of the most important ways you can get rid of your prejudices is by gaining knowledge. Educate yourself. Learn about schizophrenia. Find out as much as you can about its symptoms, its potential impact on the life of your loved one, and how you can make the best of it. This guide is a great start! The more you can learn about schizophrenia, the more you can do to help.
Talk to healthcare specialists. Read books and watch educational videos. Look up the websites of well-known health organizations and caregiver associations for valuable information. Although schizophrenia is still somewhat taboo, there are many great resources that you can use to learn more about the disease.
Learning about the disease will give you power. It will give you the confidence you need to navigate through the hardships of caring for someone with schizophrenia. Understanding the disease will also help you work out a strategy on how to deal with it.
Recommended reading
• World Health Organization
https://www.who.int/news-room/ fact-sheets/detail/schizophrenia
• American Psychiatric Association
https://www.psychiatry.org/ patients-families/schizophrenia
•EUFAMI (European Federation of Associations of Families of People with Mental Illness)
http://eufami.org
•Global Alliance of Mental Illness Advocacy Networks-Europe (GAMIAN-Europe)
https://www.gamian.eu
See the person and not the illness
Despite all the challenges that schizophrenia induces, it is essential not to dismiss the person behind the illness. Focus on the positive. Mental illness is only a part of someone’s larger picture. Beyond the symptoms and daily struggles, the person you care for is still the person you know – your parent, sibling, or loved one, who is now battling an undermining illness. It is also important not to confuse symptoms with personality traits, or the inability to act with the lack of willpower. As the illness changes the way they think and perceive the world, people with schizophrenia may not find certain aspects of life as important as before.
Withstand external prejudice
When faced with prejudices in your close environment – family members, friends, or colleagues – there are four strategies that you can use to deal with them. However, keep in mind that some of these strategies may not be beneficial in the long term.
SOCIAL WITHDRAWAL
Once the diagnosis of schizophrenia has been established, your first reaction may be to withdraw from all social activities and focus only on the person you care for. This can have many reasons, from feelings of shame and wishing to avoid stigmatizing people, to believing that you are able to do this alone. Whatever the reason, by choosing to do so, you reduce the very important social support of family and close friends. This will inevitably increase your burden.
CONCEALMENT
It is understandable that you may wish to keep the diagnosis a secret in particular social plights. However, this can lead to the fear of being discovered and feelings of shame when your secret is revealed. With that said, it is your right to decide who in your close environment should know or not about the illness, and how much information you want to share. Consider the advantages and disadvantages in each particular case.
ORGANIZING ENCOUNTERS
A significant barrier to eradicating social stigma is the fact that people rarely come into contact with stigmatized individuals, leading to a lack of empathy.
Even when contact does happen, it often involves stereotypical representations of people with mental illness – for example, interacting with a homeless person with a disorganized speech on the street –, which only reinforces the negative associations. However, things change when the contact occurs in conditions of relatively equal power and status. For example, imagine you invite a couple of close friends over for dinner, and they have the chance to talk to your loved one, who has schizophrenia.
This type of interaction is far more likely to generate positive attitudes and reduce stigma. The more frequent these interactions are, the more they are able to reduce the negative perceptions of stigmatized individuals. They are also an excellent opportunity to change the myths surrounding schizophrenia and mental illness in general.
EDUCATION
The most important measure in dealing with stigma is to educate people from your personal environment who express stigmatizing attitudes. Tell them what the disease entails, how it affects the person you care for, and what treatments are necessary. As stigma affects not only those with schizophrenia but also their families and caregivers, tell them what it means for you to take care of someone with schizophrenia. The more mental illness remains hidden, the more people think it must be something to be ashamed of. Do not forget, however, to make sure your loved one is OK with you talking to others about their condition. Even in educational conversations, you can vary the depth of information depending on how much you want to share. Try to avoid overly technical terms and make sure to keep the conversation friendly. Also, try to be empathic and to understand their point of view. Remember, their prejudices may not be ill-conceived, but rather due to being uninformed.
References
- Economou M, Bechraki A, Charitsi M. The stigma of mental illness: A historical overview and conceptual approaches. Psychiatriki. 2020 Jan-Mar;31(1):36-46. Greek, Modern. doi: 10.22365/ jpsych.2020.311.36. PMID: 32544075.
- Hatzenbuehler, Mark L. Structural stigma: Research evidence and implications for psychological science. The American psychologist vol. 71,8 (2016): 742-751. doi:10.1037/amp0000068
- Kobau R, Zack MM, et al. Attitudes toward mental illness: results from the Behavioral Risk Factor Surveillance System. Mental Health Program, United States. Substance Abuse and Mental Health Services Administration., editors. 2012; Available from: https://stacks.cdc.gov/view/cdc/22179
- Maharjan S., Panthee, B. Prevalence of self-stigma and its association with self-esteem among psychiatric patients in a Nepalese teaching hospital: a cross-sectional study. BMC Psychiatry 19, 347 (2019). https://doi.org/10.1186/s12888-019-2344-8
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011 Dec;199(6):445-52. doi: 10.1192/ bjp.bp.110.083733. PMID: 22130746.
- Miller, Del D. Atypical antipsychotics: sleep, sedation, and efficacy. Primary care companion to the Journal of clinical psychiatry vol. 6,Suppl 2 (2004): 3-7
- Harrow M. Do Patients with Schizophrenia Ever Show Periods of Recovery? A 15-Year Multi-Follow-up Study. Schizophrenia Bulletin vol. 31 no. 3 pp. 723–734, 2005 doi:10.1093/schbul/sbi026
Мифы и правда Мифы и правда о шизофрении
Как отличить правдивую информацию о шизофрении от вымысла? Разберемся вместе Как отличить правдивую информацию о шизофрении от вымысла? Разберемся вместе
далее…Кратко о шизофрении Кратко о шизофрении
ЦЕЛЬ ЭТОЙ КНИГИ — предоставить рекомендации о том, как помочь близкому человеку улучшить его жизнь и научиться справляться с повседневными проблемами, ЦЕЛЬ ЭТОЙ КНИГИ — предоставить рекомендации о том, как помочь близкому человеку улучшить его жизнь и научиться справляться с повседневными проблемами,
далее…